This information was adapted from the National Eye Institute to help patients and their families search for general information about cataracts.
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of diabetes. All can cause severe vision loss or even blindness.
Diabetic eye disease may include:
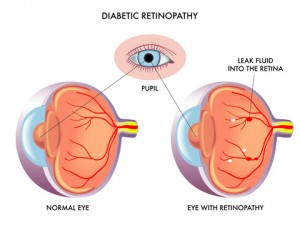
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in American adults. It is caused by changes in the blood vessels of the retina.
In some people with diabetic retinopathy, blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina. The retina is the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision.
If you have diabetic retinopathy, at first you may not notice changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
Diabetic retinopathy has four stages:
Blood vessels damaged from diabetic retinopathy can cause vision loss in two ways:
All people with diabetes–both type 1 and type 2–are at risk. That’s why everyone with diabetes should get a comprehensive dilated eye exam at least once a year. The longer someone has diabetes, the more likely he or she will get diabetic retinopathy. Between 40 to 45 percent of Americans diagnosed with diabetes have some stage of diabetic retinopathy. If you have diabetic retinopathy, your doctor can recommend treatment to help prevent its progression.
During pregnancy, diabetic retinopathy may be a problem for women with diabetes. To protect vision, every pregnant woman with diabetes should have a comprehensive dilated eye exam as soon as possible. Your doctor may recommend additional exams during your pregnancy.
If you have diabetes, you should get a comprehensive dilated eye exam at least once a year.
does diabetic retinopathy have any symptoms?
Often there are no symptoms in the early stages of the disease, nor is there any pain. Don’t wait for symptoms. Be sure to have a comprehensive dilated eye exam at least once a year.
During the first three stages of diabetic retinopathy, no treatment is needed, unless you have macular edema. To prevent the progression of diabetic retinopathy, people with diabetes should control their levels of blood sugar, blood pressure, and blood cholesterol.
Proliferative retinopathy is treated with laser surgery. This procedure is called scatter laser treatment. Scatter laser treatment helps to shrink the abnormal blood vessels. Your doctor places 1,000 to 2,000 laser burns in the areas of the retina away from the macula, causing the abnormal blood vessels to shrink. Because a high number of laser burns are necessary, two or more sessions usually are required to complete treatment. Although you may notice some loss of your side vision, scatter laser treatment can save the rest of your sight. Scatter laser treatment may slightly reduce your color vision and night vision.
Scatter laser treatment works better before the fragile, new blood vessels have started to bleed. That is why it is important to have regular, comprehensive dilated eye exams. Even if bleeding has started, scatter laser treatment may still be possible, depending on the amount of bleeding.
If the bleeding is severe, you may need a surgical procedure called a vitrectomy. During a vitrectomy, blood is removed from the center of your eye.
Macular edema is treated with laser surgery. This procedure is called focal laser treatment. Your doctor places up to several hundred small laser burns in the areas of retinal leakage surrounding the macula. These burns slow the leakage of fluid and reduce the amount of fluid in the retina. The surgery is usually completed in one session. Further treatment may be needed.
A patient may need focal laser surgery more than once to control the leaking fluid. If you have macular edema in both eyes and require laser surgery, generally only one eye will be treated at a time, usually several weeks apart.
Focal laser treatment stabilizes vision. In fact, focal laser treatment reduces the risk of vision loss by 50 percent. In a small number of cases, if vision is lost, it can be improved. Contact your eye care professional if you have vision loss.